There is a possibility that an outdated UTI medicine currently used to treat infections has another function.
In a recent case report, doctors in California state that they utilized it to treat a brain-eating amoeba infection. Even though the infection is extremely uncommon, it is nearly always lethal.
MRIs Reveal New Brain Lesions
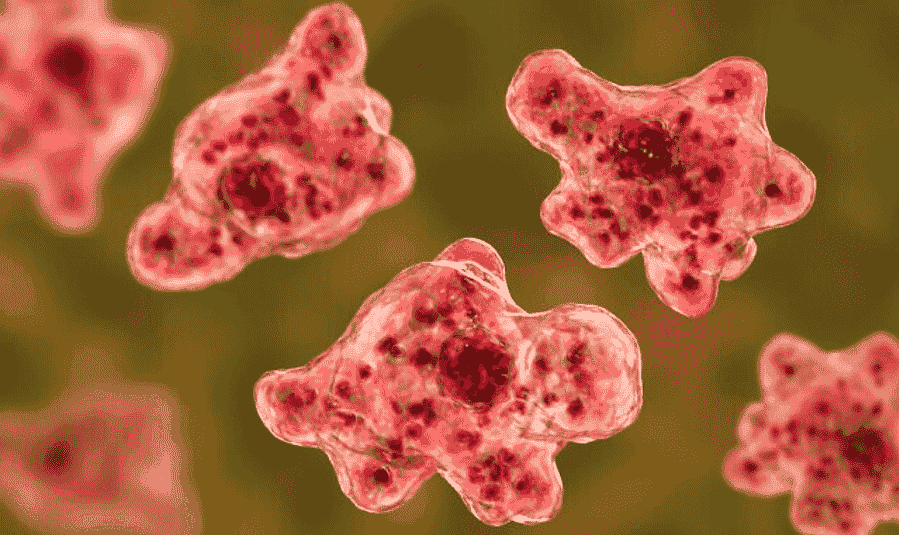
The insect that consumes the brain is known as Balamuthia mandrillaris. It is a single-celled, free-living amoeba found in soil and water nearly everywhere. In these conditions, it most likely feeds on a smaller amoeba, but it was initially discovered in the brain of a deceased mandrill monkey in the late 1980s.
In 1993, it was determined to be a different species of amoeba and one of the few capable of causing severe brain infections in humans.
The amoeba can enter the body through the nose or skin wounds, eventually reaching the brain via the bloodstream to cause granulomatous amebic encephalitis or GAE.
Unlike flesh-eating bacteria, which is a misnomer, B. mandrillaris appears to consume our brain tissue, although a significant portion of the damage it wreaks is also caused by our immune system.
Prior to the onset of symptoms such as fever, headaches, seizures, and alterations in behavior, infected individuals may be unaware of their condition for years.
However, once they do, the fatality rate is over 90%. Fewer than 200 cases of B. mandrillaris-caused GAE have been documented globally since its discovery, but everyone, including individuals with healthy immune systems, is susceptible.
In August 2021, a 54-year-old man entered a Northern California hospital after experiencing a seizure, as described in the journal Emerging Infectious Diseases last month.
Soon after initial therapy, MRI scans detected tumors and edema on the left side of his brain, and he was sent to the University of California, San Francisco (UCSF) Medical Center. Initial investigations ruled out bacterial and fungal causes, and he was eventually released from the hospital.
The doctors opted to examine the man’s biopsy samples for a suspected amoeba infection after a second examination of his case. Finally, around one month after his original visit, the test was positive for B. mandrillaris, prompting the man’s readmission to the hospital.
MRIs revealed fresh brain lesions, and he has prescribed the only known conventional treatment for GAE, a protracted combination of antimicrobials. Initially, he appeared to improve, as the size of his lesions decreased, but the toxicity of the drugs made it impossible to continue treatment.
Despite the specialists’ efforts to identify a successful and safe medicine combination, his health worsened once more.
The doctors desperately searched the medical literature for an alternative treatment. They discovered lab data conducted by their UCSF colleagues that revealed nitroxoline could be an effective anti-amoeba therapy.
After gaining approval from the man’s family and the Food and Drug Administration, the doctors began administering nitroxoline to him approximately 100 days after his initial hospitalization.
Read more: Microsoft launches new Bing powered by ChatGPT to some customers; What you need to know?
Nitroxoline Helps Man With Brain-Eating Amoeba

Despite initial kidney issues (perhaps linked to the medication), he began to improve. His brain lesions diminished after a week of treatment, and he was eventually freed from the hospital.
Nitroxoline has been licensed and used to treat urinary tract infections for many years. However, it is not commercially available in the United States, so the doctors had to obtain a supply from a Chinese pharmaceutical company exploring its potential use as a bladder cancer treatment, according to Science Magazine.
New screening methods, such as those developed by some of the co-authors at UCSF, could one day make detection easier for these uncommon cases.
The patient has had to deal with a few difficulties, but his lesions have continued to diminish and he has recovered substantially, according to the doctors. Currently, he is using a cocktail of medications, including nitroxoline, but his outpatient team intends to wean him off of them within a year.
The UCSF team reports that they have collaborated with other physicians to treat a second instance of brain-eating B. mandrillaris with nitroxoline, with similar initial success. In addition, they seek to encourage the Centers for Disease Control and Prevention to establish a local emergency drug stockpile.
Read more: $3 Epilepsy drug may cure autism symptoms, scientists discover

